It has been quite some time since I lasted blogged and boy have those months been busy! Amongst other things we’ve celebrated a 16th birthday, survived the onslaught of BTEC and GCSE exams – as well as nearly all the results – some big changes at work and a performance in the West End by G and M. With so much going on, it’s been difficult to find time to put the proverbial pen to paper, but having just come back from an amazing 10 days in Italy, I was determined to find 5 minutes wherever I could to share our travel experiences.
 Unusually, I didn’t do as much research on safe places to eat before we travelled as I have in the past, but having seen how well Italy accommodates those on special diets on our quick jaunt there a few years’ ago, I was hopeful we might have reasonable success. And so we did. With a little light touch internet searching on the ground to assist us, we found some amazing places to eat.
Unusually, I didn’t do as much research on safe places to eat before we travelled as I have in the past, but having seen how well Italy accommodates those on special diets on our quick jaunt there a few years’ ago, I was hopeful we might have reasonable success. And so we did. With a little light touch internet searching on the ground to assist us, we found some amazing places to eat.
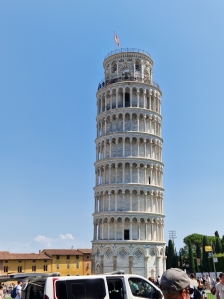
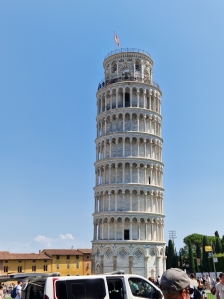
Our journey started in Pisa where we walked to see the Leaning Tower before heading for a quick pit-stop in Florence for lunch, and finally on to a beautiful farmhouse just outside Orvieto, where we spent the first week of our holiday. We didn’t eat out much whilst we were there, but the meals we did have were brilliant:
 Hard Rock Cafe Florence: A holiday simply wouldn’t be a holiday without lunch at the local Hard Rock Cafe. I can’t say we go as far as planning our destinations around the HRC locations, but it is pretty much always one of the first things M asks about once he knows where we’re going. The Italian approach to allergy-friendly eating was a little different than we’re used to, with no separate menus, but we did have an extremely knowledgeable server who was able to tell both G and M if their selections were safe or not. G picked the BBQ pulled pork sandwich, whilst M chose a starter of chicken wings, followed by the grilled chicken sandwich. Their plates were cleared in the usual fashion when we eat at a HRC and I’m told that the gluten-free bread rolls were the best that they’ve eaten anywhere in the world.
Hard Rock Cafe Florence: A holiday simply wouldn’t be a holiday without lunch at the local Hard Rock Cafe. I can’t say we go as far as planning our destinations around the HRC locations, but it is pretty much always one of the first things M asks about once he knows where we’re going. The Italian approach to allergy-friendly eating was a little different than we’re used to, with no separate menus, but we did have an extremely knowledgeable server who was able to tell both G and M if their selections were safe or not. G picked the BBQ pulled pork sandwich, whilst M chose a starter of chicken wings, followed by the grilled chicken sandwich. Their plates were cleared in the usual fashion when we eat at a HRC and I’m told that the gluten-free bread rolls were the best that they’ve eaten anywhere in the world.
Antica Cantina, Orvieto : Our base for the week, La Grande Quercia, was a fabulous farmhouse found on top of a hillside overlooking the cliff-top city of Orvieto and mid-week we decided to venture there for an explore and a lunch at the Antica Cantina restaurant. There were some great local specialities on the menu and M was delighted to learn that all of their pasta dishes could be made gluten- and dairy-free. The children started with a plate of parma ham and melon before G enjoyed a platter of goats’ cheeses with gluten-free bread and salad, and M selected the rigatoni with a tomato and smoked bacon sauce. Mike and I also chose regional dishes and we all very much enjoyed our first proper Italian meal out.
: Our base for the week, La Grande Quercia, was a fabulous farmhouse found on top of a hillside overlooking the cliff-top city of Orvieto and mid-week we decided to venture there for an explore and a lunch at the Antica Cantina restaurant. There were some great local specialities on the menu and M was delighted to learn that all of their pasta dishes could be made gluten- and dairy-free. The children started with a plate of parma ham and melon before G enjoyed a platter of goats’ cheeses with gluten-free bread and salad, and M selected the rigatoni with a tomato and smoked bacon sauce. Mike and I also chose regional dishes and we all very much enjoyed our first proper Italian meal out.
Trattoria del Buongusto, Marmore : Our one big day trip out was to the awe-inspiring Marmore Falls, the tallest man-made waterfall in the world. We spent our time exploring the various trails and climbing to get the most amazing views of all 3 tiers of the falls. We managed to buy a very basic hot dog lunch at the Falls themselves as there were no allergy-friendly options on offer, but our dinner at the nearby Trattoria del Buongusto more than made up for a somewhat scrappy lunch. Disappointingly they didn’t have any gluten-free pasta available the evening we were there, but our waitress was brilliant and helped translate the menu for us as well as letting us know which dishes could be prepared gluten- and dairy-free. This time G chose a cold meats and cheeses platter with salad and potatoes, whilst M feasted like a king on a mixed seafood platter starter followed by a mixed grill entree.
: Our one big day trip out was to the awe-inspiring Marmore Falls, the tallest man-made waterfall in the world. We spent our time exploring the various trails and climbing to get the most amazing views of all 3 tiers of the falls. We managed to buy a very basic hot dog lunch at the Falls themselves as there were no allergy-friendly options on offer, but our dinner at the nearby Trattoria del Buongusto more than made up for a somewhat scrappy lunch. Disappointingly they didn’t have any gluten-free pasta available the evening we were there, but our waitress was brilliant and helped translate the menu for us as well as letting us know which dishes could be prepared gluten- and dairy-free. This time G chose a cold meats and cheeses platter with salad and potatoes, whilst M feasted like a king on a mixed seafood platter starter followed by a mixed grill entree.




















 ill effects during our time away. It was fantastic to see a wide selection of different flavoured dairy-free ice-creams readily available in the hypermarket, although I wish we’d been able to find a good coconut ice-cream for M to try as well as the others.
ill effects during our time away. It was fantastic to see a wide selection of different flavoured dairy-free ice-creams readily available in the hypermarket, although I wish we’d been able to find a good coconut ice-cream for M to try as well as the others.


 I headed to the freezer to see what I could find and struck proverbial gold. They might not have stocked vegan magnums, but instead I stumbled across the fantastically named “Bikini 1969”, a gluten- and dairy-free ice-cream sandwich bar. Needless to say, both G and M were quick to take up my offer to try this treat – their first ice-cream sandwiches ever – and what a hit it was. We didn’t quite make it back there every day, but we did partake of an ice-cream from the Magnum pleasure store more than once during our stay.
I headed to the freezer to see what I could find and struck proverbial gold. They might not have stocked vegan magnums, but instead I stumbled across the fantastically named “Bikini 1969”, a gluten- and dairy-free ice-cream sandwich bar. Needless to say, both G and M were quick to take up my offer to try this treat – their first ice-cream sandwiches ever – and what a hit it was. We didn’t quite make it back there every day, but we did partake of an ice-cream from the Magnum pleasure store more than once during our stay.
 All of the ice-creams were clearly marked with the red scoops depicting those flavours that were safe for vegans and therefore for our dairy-free duo. What was fantastic was that there was a great mix of traditional ice-cream flavours, fruit sorbets and some more unusual ones for us to try and they all tantalised the taste-buds. I can’t quite remember all of the flavours we tried between us, but I know chocolate orange, fig, peach and lime were amongst them. Once again it was fantastic to see G and M experiencing being able to order a gluten-free cone filled with 2 scoops of their choice of an array of safe ice-cream flavours, something they’ve never been able to do before.
All of the ice-creams were clearly marked with the red scoops depicting those flavours that were safe for vegans and therefore for our dairy-free duo. What was fantastic was that there was a great mix of traditional ice-cream flavours, fruit sorbets and some more unusual ones for us to try and they all tantalised the taste-buds. I can’t quite remember all of the flavours we tried between us, but I know chocolate orange, fig, peach and lime were amongst them. Once again it was fantastic to see G and M experiencing being able to order a gluten-free cone filled with 2 scoops of their choice of an array of safe ice-cream flavours, something they’ve never been able to do before.














 Unusually, I didn’t do as much research on safe places to eat before we travelled as I have in the past, but having seen how well Italy accommodates those on special diets on our
Unusually, I didn’t do as much research on safe places to eat before we travelled as I have in the past, but having seen how well Italy accommodates those on special diets on our  Hard Rock Cafe Florence
Hard Rock Cafe Florence
